Pain is individual: Towards personalised therapy
One small slip while chopping onions and here we go: Sensory neurones surrounding the wound are activated. An electrical signal then races along the neural pathways of the arm into the spinal cord and from there into the thalamus, the cortex and other parts of the brain. Within milliseconds, the pain signal has reached our consciousness and we ruefully hold our bleeding finger.
As unpleasant as it is, pain is vital, emphasises Manuela Schmidt, Head of the Systems Biology of Pain research group at the University of Vienna, who we are visiting in the lab today, "Those who know no pain lead a dangerous life: Persons who are insensitive to pain from birth due to a rare genetic mutation do not notice injuries and usually have a short life expectancy." Therefore, acute pain is our friend: It works like an alarm bell, prompting us to treat the wound and be more careful next time. Or to go to the doctor.
When the pain does not stop
If this alarm bell rings continuously for more than three months, this is referred to as chronic pain. During the transition from acute to long lasting pain, known as chronification, the body plays a trick on itself, explains the expert, "If the nervous system is constantly activated by a pain stimulus over a longer period of time, it becomes over-sensitised at some point: The pain is stored in a kind of 'memory' and recalled again and again."
In most cases, we can no longer detect physical damage or injuries at this point. This is one of the reasons why people suffering from chronic pain are often additionally subject to stigmatisation.
The biochemist Manuela Schmidt was a postdoctoral researcher in the research group of the Nobel Prize laureate in medicine Ardem Patapoutian at the Scripps Research Institute in La Jolla, California. There, she conducted research on molecules that play a central role in the perception of pain and touch. During this time her fascination with the biology of pain developed. But the researcher's commitment is also a result of witnessing hardship in her family. One of her parents suffers from chronic pain and Manuela Schmidt experienced first-hand the vicious cycle of subsequent problems associated with this diagnosis.
Together with her highly motivated team, she is now doing everything she can to understand how certain protein networks influence pain in different phases of life and, in particular, in different genders. The researchers pursue a holistic approach: systems biology, which focusses on complex biological networks and interactions instead of just concentrating on individual molecules. This opens new avenues for the development of more targeted and individualised therapies.
Pain research at a glance
For a long time, researchers considered pain a concomitant symptom of other diseases. Pain has only been taken seriously as an independent field of research since the 20th century. As pain is a complex and individual phenomenon, the effectiveness of universal medication is very limited. New insights into specialised pain receptors, genetic factors and molecular mechanisms in chronic pain are now suggesting novel opportunities for targeted therapies. However, it is a long way to go before today's research can be translated into a safe drug that is ready for the market.
Chronic pain is a disease
Meanwhile, many people are waiting for these therapies: Estimates suggest that one in five people in Europe are affected by chronic pain, an even higher prevalence than conditions like diabetes or asthma. To illustrate this: In Austria, there are around 1.8 million people who suffer from chronic back pain or migraine. Associated consequences, such as depression, can be so severe that it impairs the person’s "work and social life and the ability to care for themselves": This is referred to as ‘high-impact chronic pain’.
“Chronic pain is a disease in its own right which has consequences for society as a whole," emphasises Manuela Schmidt. For example, a recent study in Germany estimates that the economic damage caused by back pain far exceeds the costs of treatment alone. As is so often the case, people who are also disadvantaged in other areas of life, e.g. due to low income or a lower education level, are more frequently affected by chronic pain than others.
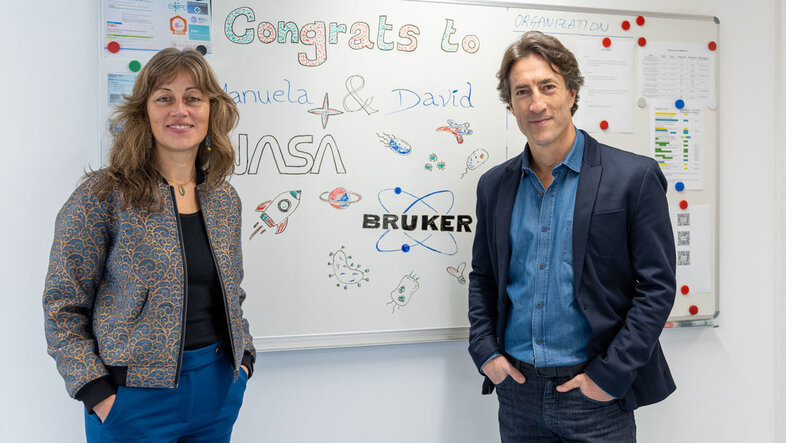
Research on the functional microbiome and metaproteome unique in Austria
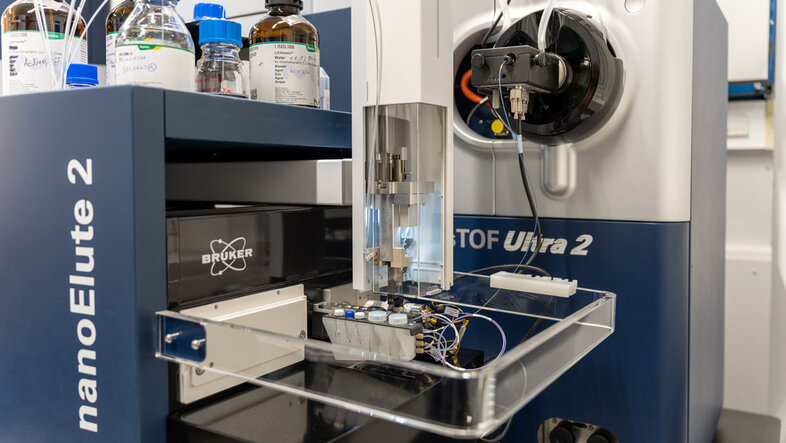
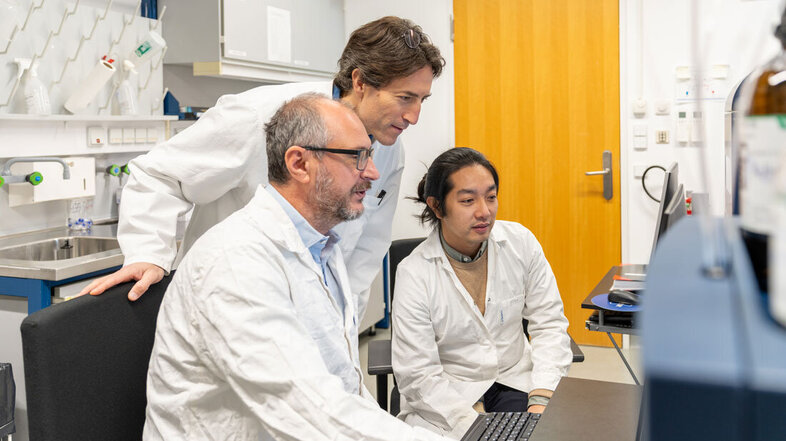
The scientist David Gómez Varela has been conducting research in the Systems Biology of Pain research group since 2021, where he heads the new Centre of Excellence for Metaproteomics, a cooperation between the University of Vienna and the Bruker company. During our tour of the laboratories of the Department of Pharmaceutical Sciences at the University of Vienna in the 9th Viennese district, he proudly presents the latest, and most expensive, addition to the team, which has emerged from the partnership with Bruker: "the timsTOF Ultra 2".
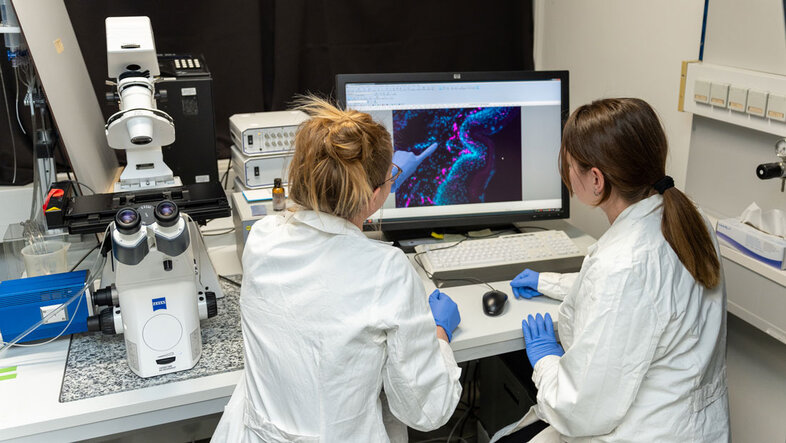
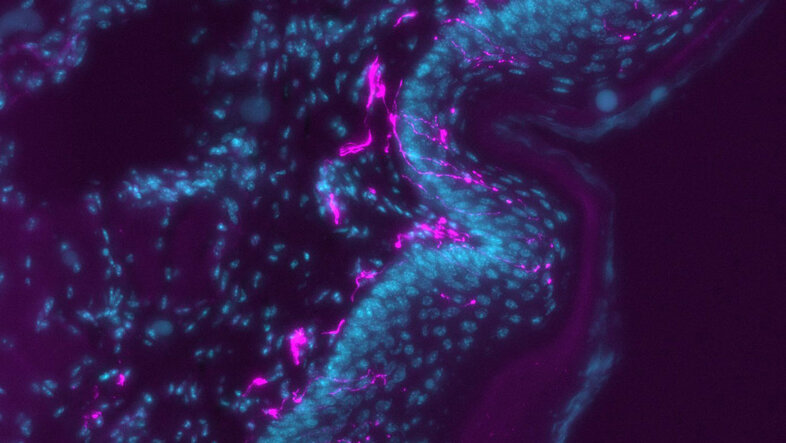
It is the most state-of-the-art mass spectrometre of its kind, "a real game-changer for our research." This machine is able to analyse the individual components of a complex protein mixture. In this way, the proteome of a biological sample, i.e. the entirety of its proteins, can be assessed. Decoding the proteome is important because certain proteins play a key role in the development of pain: They act as molecular switches that trigger and transmit painful signals.
Proteome research is key for new active substances
This modern technology allows researchers to focus on another important piece of the puzzle in the complex system of pain: the microbiome. Schmidt and Gómez Varela's team are not only studying the microorganisms that live in and on us, but also their activities and tasks (the functional microbiome) and proteins produced by these microbes (the metaproteome). Investigating the metaproteome reveals how these proteins contribute to the health or function of an organism, how microbes interact with each other and which metabolic processes are involved.
"Our latest findings strongly suggest that gut microbes play a key role in how proteins, hormones and the immune system work together in the body," explains Gómez Varela. "This interaction between microorganisms and host is largely unexplored, changes over time and cannot be explained by genetics alone. This is why we conduct our microbiome and pain research at a systems biology level in order to see the bigger picture. With our technology and expertise, we can investigate more precisely than ever before, at the proteome level, how the functions of these microorganisms influence chronic pain and other diseases."
Small building blocks, big impact
- Systems biology: Systems biology investigates how different parts of an organism, such as genes, proteins and cells, work together to make life possible.
- Proteome: The proteome comprises all proteins of an organism, tissue or cell at a certain point in time. Proteins control many life processes.
- Microbiome: The microbiome encompasses all microorganisms (e.g. bacteria and fungi) that live in and on a living organism, such as in the gut or on the skin.
- Metaproteome: The metaproteome is the entirety of proteins produced by all microorganisms in a microbial community. It is the ‘proteome of microbes’, so to speak.
- Functional microbiome: The functional microbiome describes the overall activities and tasks of the microorganisms in the microbiome, such as the production of nutrients and supporting the health of their host but also driving pathologies.
Using this approach, the researchers hope to pave the way for new painkillers. They are needed because common substances such as opioids many have side effects beyond their abuse potential. because opioid receptors are involved in many different processes in the body. The aim would be to develop medications that target only those molecules and signalling pathways that are specific to the pain condition in question. In order to develop such customised therapies, it is necessary to understand the exact molecular processes and differences between acute and chronic pain.
However, what the research team manages to unlock from the secrets of the metaproteome could also prove useful for other medical applications. "We regularly find thousands of new peptides, which are small proteins that are produced by gut microbes and may act like natural antibiotics," says Gómez Varela enthusiastically. "We now have to test these peptides for their suitability as active substances in further experiments. Cooperation between science and industry, such as our collaboration with Bruker, is crucial for this. Vienna is an ideal location: Here, we have leading pharmaceutical companies and committed funding bodies that can push these innovations."
Personalised pain medicine is the future
Another aim of the researchers is to focus more than ever on individual differences. Just like private individuals can have their genomes analysed today, the team is developing a technology to decode changes in a person's functional microbiome using stool samples that can be easily sent in for analysis. This will provide more precise results than currently available microbiome tests.
For Manuela Schmidt, personalisation is also the future of pain medicine. Until now, research has often neglected differences between people. For example, for a long time, we have lacked knowledge about women-specific symptoms and disease progression. Among other things, this has led to a data gap in gender medicine.
This neglect persists even though pain is demonstrably highly individual: Each of us experiences the above-mentioned incident with the onion and the kitchen knife differently. This is due to individual differences in proteins and signalling pathways that act as pain receptors or transmitters. Moreover, their quantity and activity fluctuate with age, hormonal balance, mental state and even the time of day.
As everyone is different, it is hardly surprising that we are also susceptible to chronic pain in different ways. This is a fact that should also be considered in diagnostics. The researchers hope to find specific proteins serving as pain biomarkers, which may be used to make chronic pain measurable on a molecular level. This would prevent situations in which the suffering of many patients is being dismissed or trivialised as purely psychological.
Biochemistry cannot solve everything
However, it is also clear that even the most innovative and dedicated research group cannot combat chronic pain on its own. "Proteins are not everything," says Schmidt, “It gets really exciting when you look at different levels of complexity simultaneously, from gene regulation to the proteome and hormone balance to metabolites. We work closely with international clinical pain experts, but we also have links with pharmaceutical research, microbiologists and network medicine at the University of Vienna."
Schmidt emphasises that we will not have a single pill for chronic pain in the future either. "Pain and the associated suffering are not purely biological phenomena, they arise from a complex interplay of physical, emotional and social influences." For example, chronic back pain does not only have physical causes. Psychological factors, such as job satisfaction, also appear to play a role. Integrative pain therapy, which should be accessible to everyone, should take this complexity into account, says Schmidt: so that pain patients are treated not only more efficiently ‒ but also more fairly.
After career stages in Würzburg, Germany, California and Göttingen, she came to the University of Vienna in 2020. She is Vice-Dean of the Faculty of Life Sciences.
He patented several techniques that enable personalised health tests using molecular signatures such as proteins, metabolites and RNA. Since moving to the University of Vienna, he has specialised in the development and application of technologies to study the gut microbiome and host responses.
- Systems Biology of Pain research group at the Department of Pharmaceutical Sciences
- Press release: opening of the Centre of Excellence for Metaproteomics at the University of Vienna in collaboration with Bruker (in German)
- Website of Manuela Schmidt
- Website of David Gómez Varela
- More information about Manuela Schmidt's participation in the NASA STAR programme
- Publication by the Systems Biology of Pain lab: taxonomic and functional characterization of host-microbiome interactions
- Publication by the Systems Biology of Pain Lab: Ultra-sensitive metaproteomics